Helpful Information for Medi-Cal Renewals
L.A. Care provides information and addresses many questions about the Medi-Cal renewal process. The Los Angeles County Department of Public Social Services (DPSS) can also be contacted at 1-866-613-3777 (TTY) 1-800-660-4026 for additional information.
Due to the continuous coverage requirement that was enacted during the public health emergency (PHE), Medi-Cal members have been able to keep their coverage regardless of any changes in circumstances. Once the continuous coverage requirement ends on March 30, 2023, the Los Angeles County Department of Public Social Services (DPSS) will resume Medi-Cal annual renewal redetermination operations on April 1, 2023.
L.A. Care’s call to action for our providers, as trusted partners to their patients, is to conduct outreach and bring awareness to resumption of Medi-Cal renewals through utilizing the following key messages recommended by DHCS:
Resources
Visit one of our Community Resource Centers offering on-site Medi-Cal enrollment and renewal assistance for members.
L.A. Care hosted a Medi-Cal Redeterminations Webinar on May 10, 2023. View the presentation deck or the recording of the webinar.
We've developed Medi-Cal Renewal Toolkits for providers. The provider toolkits list resources that providers can utilize to educate and inform members during point of contact visits on the renewal resumption process, to ensure continuity of coverage and avoid gaps in coverage.
 L.A. Care Toolkit for Providers
L.A. Care Toolkit for Providers
 Street Medicine Toolkit for Providers: Medi-Cal Redetermination
Street Medicine Toolkit for Providers: Medi-Cal Redetermination
Also, the following resources can be used for display in offices and to educate and inform members on the Medi-Cal renewal process. All of the PDF files offer information in all threshold languages.
 L.A. Care flyers for patients
L.A. Care flyers for patients L.A. Care posters
L.A. Care posters Plan Partners flyers for patients
Plan Partners flyers for patients Plan Partners poster
Plan Partners poster MediCal Keep Your Coverage Flyers
MediCal Keep Your Coverage Flyers
The Los Angeles County Department of Public Social Services also has a BenefitsCal guide, which has written instructions on the Medi-Cal renewal process. Frequently asked questions and answers are below, along with the following videos about important steps to take.
Additional Member Support
Members who need help with accessing their Medi-Cal coverage, who received notice their Medi-Cal was discontinued, or have any additional coverage questions, should contact the Los Angeles County Department of Public Social Services at 1-866-613-3777 (TTY) 1-800-660-4026, go to benefitscal.com or visit KeepMediCalCoverage.org for more information and to sign up for text or email updates on Medi-Cal renewals.
Every 12 months, DPSS will conduct a review of a Medi-Cal member's information to determine if they are still eligible to continue receiving Medi-Cal benefits.
Yes. It is important that members respond to county requests for updated information, including renewal packets. The member does not need to return the paper annual renewal form but they must provide the necessary information requested in the form and sign the form through any of the available means indicated.
Members need to read the pre-populated information, if it is wrong, they need to make changes or updates on the renewal form. They will need to give proof when the renewal instructs them to. If they get income, they need to give proof. The renewal form lists examples, which include pay stubs and tax returns.
Members DO NOT need to complete the section about non-income assets and property or give proof.
The renewal form has all the information Medi-Cal knows about a member. Members gave most of the information in previous applications and renewals. Some of the information may come from other places Medi-Cal has access to, including:
- Social Security
- Employment Development Department
Yes. If a member needs assistance completing their renewal packet, there are agencies across Los Angeles County with bilingual staff who are able to provide Medi-Cal enrollment assistance. You can view the list of available agencies here.
The following Community Resource Centers (CRC) listed below are currently offering assistance with Medi-Cal enrollment and renewals:
Palmdale
2072 E. Palmdale Blvd., Palmdale, CA 93550
213-438-5580
El Monte
3570 Santa Anita Ave, El Monte, CA 91731
213-428-1495
Pomona
696 W. Holt Avenue, Pomona, CA 91768
909-620-1661
Metro Los Angeles
1233 S. Western Avenue, Los Angeles, CA 90006
213-428-1457
Lynwood
3200 East Imperial Hwy, Lynwood, CA 90262
310-661-3000
East Los Angeles
4801 Whittier Blvd., Los Angeles, CA 90022
213-438-5570
Norwalk
11721 Rosecrans Avenue, Norwalk, CA 90650
562-651-6060
Wilmington
911 North Avalon Blvd., Wilmington, CA 90744
213-428-1490
Long Beach
5599 Atlantic Avenue, Long Beach, CA 90805
562-256-9810
Inglewood
2864 W. Imperial Hwy, Inglewood, CA 90303
310-330-3130
Panorama City
7868 Van Nuys Blvd, Panorama City, CA 91402
213-438-5497
West Los Angeles
11173 W. Pico Blvd, Los Angeles, CA 90064
310-231-3854
If an individual needs help completing their Medi-Cal application or renewal packet, they can call a CRC to schedule an appointment with an application assister.
- The annual renewal month is the month in which the member's annual renewal is due. Typically, the annual renewal due month is the 11th month after their application month.
- Members will receive a letter in the mail indicating when their renewal is due.
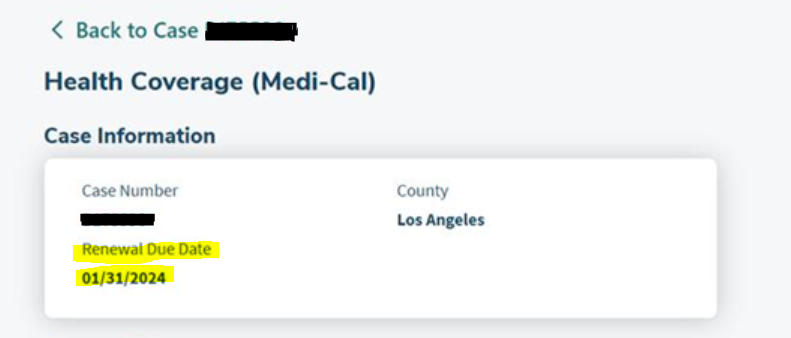
- Members can also find their renewal due date information online by logging in or creating an online account at https://benefitscal.com/ and linking their Medi-Cal case. The renewal due month will be listed in the member’s account under ‘Case Information’. Members can also call DPSS at 1-866-613-3777 Monday – Friday from 7:30 a.m. – 6:30 p.m. (excluding holidays) to request this information.
DPSS will attempt to verify the member's information through multiple sources available to the county. If DPSS locates the information needed to redetermine eligibility through the ex parte process, DPSS will complete the annual renewal and send the approval Notice of Action letter.
- An annual renewal form will be sent to the member if DPSS is unable to redetermine continued Medi-Cal eligibility through the ex parte process.
- Members who do not have a valid social security number will not be able to successfully complete the ex parte process and a packet will be sent to have the beneficiary complete their annual Medi-Cal renewal.
- Members who receive a renewal packet must complete it and turn in the extra information it requests. This must be done in order for the member to keep their Medi-Cal coverage.
DPSS will only ask for the information they need and for things that affect each individual member’s Medi-Cal coverage. They will need details and proof of any changes, to include whether a member:
- Gets married or divorced
- Has a child, adopts or places a child for adoption
- Becomes pregnant
- Gets more or less money
- Gets any other health coverage, like through a job or Medicare. This won't stop their Medi-Cal
- Moves, or changes who is living in their home
- Has become disabled or had a change in their disability
- Has a change in how they file their income taxes, such as starting or stopping claiming someone as a tax dependent
- Has a change in citizenship or immigration status
- Are incarcerated (jail, prison, etc.) or released from incarceration
- Has a change in American Indian or Alaska Native status
- Has a change in their tribal status
- Changes their name, date of birth or Social Security Number (SSN)
- Has any other changes that may affect their income or household size
If a member gets income, they may need to give proof. The form lists examples such as pay stubs and tax returns.
Members do not need to tell DPSS about non-income assets, which include bank accounts, homes and vehicles.
- Members do not need to turn in proof of their assets and property
- Members do need to report:
- If a new person with property moves in
- If they get money from their property (e.g. rent payments)
If a member does not have money, they can simply complete a sworn statement to DPSS that they do not have income or money.
Yes. The packet from DPSS will arrive in a yellow envelope.
The member is provided 60 days to provide the requested information to DPSS. If the requested information is not received by the 60-day due date, Medi-Cal benefits will discontinue at the end of the renewal due month.
DPSS will review the member’s renewal and determine if they are still eligible to get Medi-Cal. If the renewal is missing something, DPSS will ask for more information and send the member a notice telling them what information they need.
If DPSS has the information they need, they will send the member a notice to tell them whether or not they still qualify for Medi-Cal coverage. If they do still qualify, the letter will indicate that their Medi-Cal is renewed for one year. If they do not still qualify, the letter will indicate when the member’s Medi-Cal coverage ends.
Members may go to their appointments; they still have Medi-Cal coverage while the county is looking at their renewal form. Coverage will only end if they are no longer eligible. If a member is no longer eligible, they will get a notice of action and it will say when their Medi-Cal will end. These members can still get care until this date.
Members have up to 90 days from the discontinuation date to provide the information needed to re-establish coverage. After 90 days, members will have to submit a new Medi-Cal application.
Requested information can be submitted by mail, in person, online, or phone. Members can submit information online by logging in or creating an online account at benefitscal.com. To submit information by phone, members can call DPSS at 1-866-613-3777 Monday – Friday from 7:30 a.m. – 6:30 p.m. (excluding holidays).
Medi-Cal members can receive alerts on their case by creating an online account at benefitscal.com.
Yes. DPSS has released a video tutorial and written instructions on the Medi-Cal renewal process. These tools can be accessed on the L.A. Care website.
Yes. DPSS will accept other forms of identification if a California ID is not available. Accepted documents include passports, bus passes or any other form of identification. As a last resort, DPSS will also accept an affidavit.
Individuals experiencing homelessness who are in need of a mailing address to receive/send communication to/from the county may utilize a county district office address closest to them. Please reference the office locations listed on the county website.
No, to maintain continuity of coverage for these individuals who would have aged out until the new law takes affect, counties have been instructed to deprioritize these renewals towards the end of the unwinding period.
- Medi-Cal is a free to low cost; all residents regardless of immigration status are eligible. The new rules start January 1, 2024.
- These members will need to renew their current coverage when they get a notice. It will continue until the end of the year.
- On January 1, 2024, they will get full-scope coverage. Their local Medi-Cal office will transfer them. They do not need to do anything. DPSS will send them a letter about their new benefits.
Individuals who have Supplemental Security Income (SSI) get Medi-Cal through the Social Security Administration. If a member has questions, please advise them to call 1(800) 772-1213, Monday – Friday, 8:00 a.m. – 7:00 p.m. or they can visit their local Social Security Office.
If a member receives SSI, they can report changes by calling 1(800) 772-1213, Monday – Friday, 8:00 a.m. – 7:00 p.m. or they can visit their local Social Security Office.
If a member gets a renewal form and does not complete it, their Medi-Cal will end.
- If it is less than 90 days from the date on the letter they can turn in their renewal form or missing information. DPSS will see if they still qualify for Medi-Cal, these members do not need to turn in a new application.
- If it is more than 90 days after the date on the letter, they must turn in a new Medi-Cal application.
The member can ask DPSS to look at their case, these members should contact DPSS. If they cannot help the member, the member can ask for a Medi-Cal Fair Hearing.
Members can submit an online request or call the State Hearings Division toll free at (800) 743-8525.
The member’s notice had a date of when their Medi-Cal ended. If they asked for a hearing before their Medi-Cal ended, they still have Medi-Cal coverage.
If a member no longer qualifies for Medi-Cal, they may be able to get health coverage through a Covered California plan and could also get financial assistance. If a member qualifies, DPSS will share their information and Covered California will enroll them in a quality plan. They will select a plan that gives the best value at the lowest cost, L.A. Care Covered.
These members should look out for important notices from Covered California. The envelope may say “Stay Covered with Covered California”. If the member gets a notice asking them to confirm their plan, they should respond right away. They will also have the option to change or cancel their plan.
For assistance with L.A. Care Covered, individuals can contact L.A. Care directly at 1-800-222-4239, visit Covered California's website, or call Covered California's service center at 1-800-300-1506.
Medi-Cal will never ask for money to turn in a renewal. If a member gets a call asking for money to complete their renewal, they can report it to the Medi-Cal fraud hotline at 1-800-822-6222.
 Community Resource Center: Renewal Assistance Flyer
Community Resource Center: Renewal Assistance Flyer Medi-Cal Redeterminations Webinar Presentation
Medi-Cal Redeterminations Webinar Presentation